In the midst of rising respiratory diseases and previously controlled diseases such as tuberculosis that make alarming comebacks, a new CDC report provides further evidence that bird flu is not detected for people.
The last Morbidity and mortality weekly reportWhose publication was delayed, describes three cases of highly pathogenic Aviaire Influenza H5N1 in American veterinarians who work with cattle, with two of the cases are missing A clear source of exposure.
None of the veterinarians has experienced the flu -like symptoms and the spread from person to human is still unnoticed, but researchers are concerned that this capacity may only have been removed a few genetic mutations.
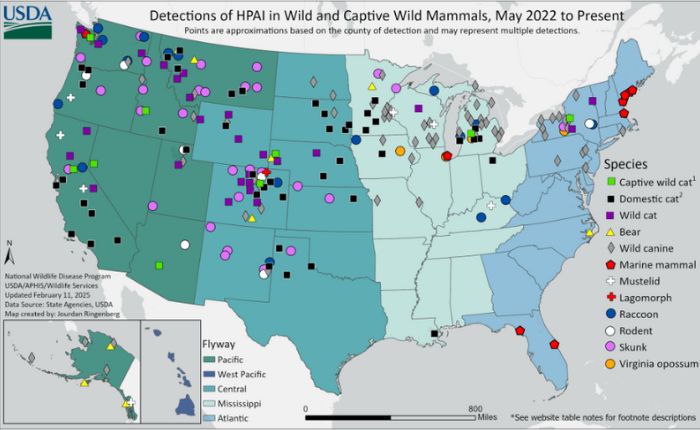
Instead, these cases were detected by antibody tests of 150 veterinarians who worked in 46 American states in September, which reveals that bird flu takes place beyond well -known infection zones. One of the vets who tested positive works with cattle in Georgia and South Carolina; Neither of the two state has fallen of bird flu in their dairy students.
“Clearly infections are happening that we miss” New York Times.
The transfer of H5N1 by cow’s milk has now been confirmed experimentally. In the light of all this, health officials urge all states to participate in the National Milk Testing Program.
https://www.youtube.com/watch?v=JFQE5HAUYDE frame order = “0 ″ all =” accelerometer; Autoplay; clipboard writing; coded media; gyroscope; Picture-in-Picture; Web-Share “ReferencerPolicy =” Strict-Origin-When-Cross-Origin “Allowfullscreen>
As with any rapidly mutering virus, every decline Incoming gives the disease more opportunities to test random mutations, so that the possibility of stumbling on a stumble that makes it possible to spread between people.
“If there are more often cases than in people detected, we run the risk of missing minor changes with which the virus can spread much more easily in people,” Lauer, researcher from the University of Nebraska, told NPR.
The first case of human H5N1 in Nevada was reported last week, so that the total known human cases were brought to 68 in the US. Nevada has also just detected a new H5N1 stem in cows mammal cells.
“An important part of stopping the transmission of viruses is to follow them,” explained Emory University -epidemiologist Jodie Guest after the first human H5N1 Dood of the US was confirmed on January 6, 2025.
But delays in sharing information because of the freezing of communication from some federal health agencies make this already challenging task even more difficult.
The deletion of CDC data already resulted in the now-drawn fears about H5N1 CAT-to-human transmissions.
Instead, KFF Health News reports dairy workers who have infected cats, probably with their work clothing, but this information still has to be released. Data from these health agencies are currently not accessible elsewhere as they could ever.
“CDC At present, no influenza data is reporting via the WHO worldwide platforms, Flunet [and] Liquid, that they have provided information [on] For many, many years, “that epidemiologist Maria van Kerkhove said in a media letter.
“We communicate with them, but we have heard nothing.”
Cases of cat-to-man transmission have occurred with older bird flu species, but none so far with H5N1. Two more pets were euthanized with the disease after eating raw pets food in Oregon.
In the meantime, health officials encourage us all to keep ourselves and pets away from raw dairy products, to avoid pets raw meat, not to interact with animals in the wild and to wear protective equipment as the handling of potentially infected cattle.
Signs of animal infection include fever, sleepiness, lack of coordination, moving in circles, a head tilt and/or an inability to stand or fly, and must be reported to the local authorities.
The CDCs Morbidity and mortality weekly report Can be read here.


